View School as a Partnership in the Midst of Pediatric Cancer - Building the Care-Team!
How can families navigating pediatric cancer begin to look at school as a partnership, as opposed to an additional burden or stressor?
Very few words bring life to a halt like pediatric cancer. When this happens, it is natural (and survival) for parents to shift their focus from school, or any other extracurricular activities, to immediately focusing on the diagnosis, treatment, survival, and cancer's lasting effects. Only time and information will bring a parent's focus back to the value of school (or anything else for that matter.)
When the pediatric cancer patient enters (or re-enters) school, it is important to educate and advocate for the needs of the pediatric cancer patient (and even their sibling). Parents can start the process by:
- Identifying Care-Team members at the school (see below visual & roles for guidance)
- Scheduling initial & follow-up Care-Team meetings
- Communicate on a bi-weekly, monthly or quarterly basis with the Care-Team
This is a short visual to help you better understand who the care team members might be:
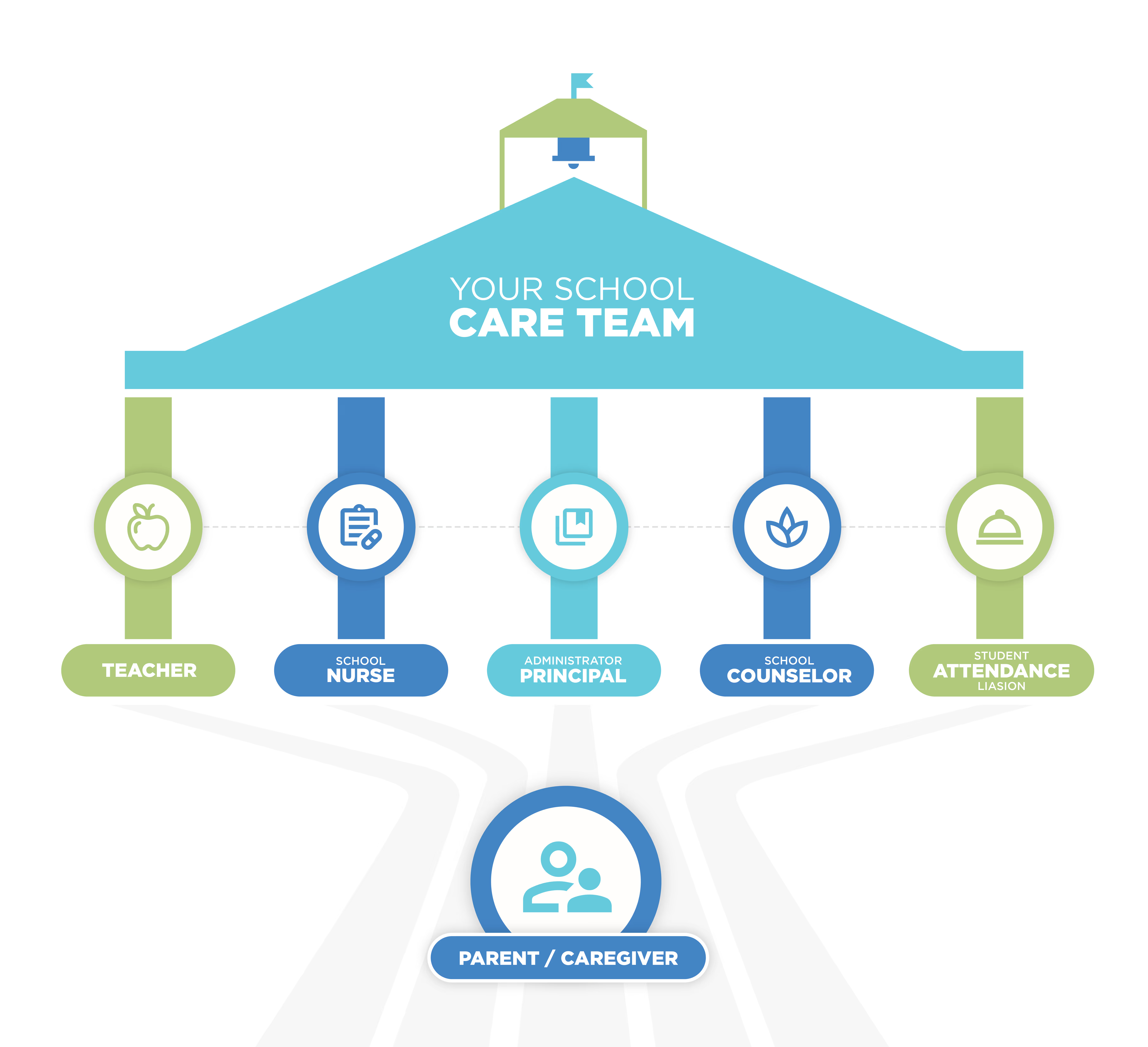
Each school personnel plays a different role, but it’s imperative that they all work together to help meet the needs of both the child with pediatric cancer and their siblings. The attention often focuses so heavily on the cancer patient that the sibling can easily (and often does) fall behind.
With that said, here is a look at each stakeholder/care-team member’s role (this can change based on each school and their personnel):
- Teacher:
- Track academic progress/deficiencies, along with missed assignments
- Help facilitate classroom discussions when/if questions arise (it is imperative that the parents work with the teacher when developing such talking points and what information they want to be communicated). For the teacher, this could be a sensitive discussion, so lean on the School Counselor when/if needed to help facilitate.
- Help maintain social connections with peers (in person or via virtual learning)
- Ensure 504 classroom accommodations are being met, or assist with the Individualized Education Plan (IEP)
- Nurse:
- Develop Individualized Health Plan (IHP) some text
- Baseline understanding of illness and treatment
- Develop an Emergency Care Plan
- Administer daily medication (when/if needed)
- Ensure IHP and EMC are being adhered to and followed
- Communication with the medical team regarding any adverse effects of treatment on educational performance (ROI will be needed to open any lines of communication)
- Develop Individualized Health Plan (IHP) some text
- School Counselor, Social Worker, and Special Education Case Manager
- 504 Coordinator & Individualized Education Plan team member
- Work with family & teacher to create and implement accommodations (if needed)
- Social and Emotional Check-In (CICO daily or weekly)
- Education/Advocacy (school-wide, grade-level, classroom, small group, or individual.
- Connect family with additional supports and resources in the community (if needed)
- Outside referrals, small group, individual counseling, food boxes, etc
- Help with transitions:
- From hospital, to home, to school
- From school to home, to hospital
- Align additional supports when/if needed:
- Virtual Learning or Homebound
- 504 Coordinator & Individualized Education Plan team member
- Student Attendance Liaison:
- Track daily attendance and doctors’ notes
- Communicate weekly with the truancy liaison
- Inform the care team (teacher, nurse, counselor, admin) of weekly attendance and upcoming extended absences
- Ensure the front office communicates with the truancy coordinator to ensure they are aware of the situation and the support in place.
- School Administrator:
- Awareness of family, child, and their student support plan
- Bi-weekly or monthly meetings with the Care Team to review any progress and changes
From a communication standpoint, parents need to decide what information is necessary. They also need to take into consideration the age and social and emotional needs of the child. The older the children get, the less information they (and the child) may want to share. For example, older children may be fearful of social isolation if their peer group finds out about the cancer diagnosis. This is understandable and common, but a baseline of information is suggested for the school to understand best and support the needs of the child and the sibling(s).
Information and insight allow for the partnership to occur, as opposed to keeping a child’s educational team at bay. Of course, a Release of Information (ROI) will need to be on file for any communication route to occur between the school and any healthcare provider.
How to initially build the Care Team:
- Identify Care Team Members (see above suggestion). The school should place one of the care team members as the lead communicator in this situation. From my professional experience, the School Counselor is often best served to fill this role.
- Schedule an initial in-person meeting with the students' Care Team. If an in-person meeting is not achievable, a Zoom meeting is suggested. Avoid any initial information to be shared via Class DoJo or email, as the severity of the need warrants a more formal meeting,
- Decide early what information the family and child feel comfortable sharing, along with any fears or worries the family and child may have (social impact, mood shifts, loss of hair, etc).
Considerations:
- Type of cancer with any educational materials for the Care Team
- Treatment schedule and any planned absences
- Potential setbacks or impacts of treatment
- Physical
- Social & Emotional
- Cognitive
- Review of potential internal support at school
- Individualized Health Plan (IHP), Emergency Care Plan, Section 504, Individualized Education Plan (IEP), etc.
- Review of potential external supports at home
- Virtual, homebound, printed materials
- Re-entry plan when transitioning to and from school
Once the educational game plan is developed, make sure each member of the Care Team is aware of their role and signs off on the support plan. Remind the care team about the fragility of the information and maintaining confidentiality and HIPAA compliance.
Lastly, during the initial in-person meeting, determine the best route for future communication. This could be a quarterly or monthly in-person meeting or even a bi-weekly conference call. As a parent, be ready to pivot and keep the care team members in the loop of any successes or setbacks.
Building the Care Team is just the beginning and know that the partnership isn’t something that subsides once the threat of pediatric cancer is over (which may never completely occur). The immediate and long-term effects of pediatric cancer warrant a lasting relationship with the current, and all future schools.
It takes a village. Always has. And always will!
About the Austin Hatcher Foundation (AHF)
AHF is dedicated to providing free mental and behavioral health therapy and unique solutions to families throughout their journey and recovery from childhood cancer. The foundation’s services encompass a wide range of support, including educational support (IEP/504 plan, tutoring and virtual learning), grief counseling, occupational therapy, family counseling, sibling tutoring, trauma therapy, industrial arts therapy and much more. With a focus on empowering families to cope in the present and thrive in the future, AHF ensures that every child and their loved ones receive the care they need.




.png)

.png)
